The “Acute Chest Syndrome” (ACS) is one of the clinical manifestations in the cardiopulmonary (heart-lung) system of people living with the sickle cell disorder. It is a vaso-occlusive crisis, characterized by low oxygen level (hypoxia), fever (at 38°C), chest pain, cough, increased rate of breathing and heart beat (dyspnoea, tachypnoea, tachycardia), leukocytosis, and lung infiltrates.
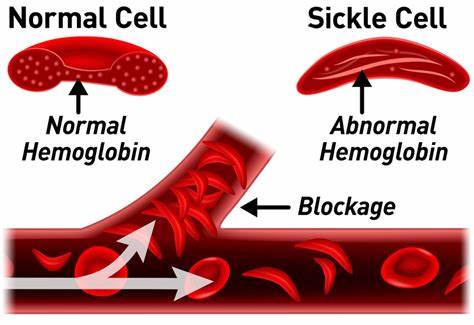
A Vaso-occlusive crisis or painful crisis, is one of the many crises sickle cell patients experience. It is initiated by the blockage of blood flow by sickled red blood cells resulting in the deprivation of oxygen to tissues.
ACS can be commonly found in people with sickle cell anaemia (HbSS), and sickle cell-beta zero thalassemia. About fifty percent of people living with sickle cell disorder, will have an ACS episode, children more commonly than in adults. The severity of this complication increases with age due to higher risks of clogged arteries by bone marrow and fat. Recurrent episodes of acute chest syndrome, can lead to other long-term lung complication such as pulmonary hypertension.
Acute Chest Syndrome, can be detected by running the following diagnostic examinations on sickle cell warriors; chest X-ray, complete cell count, reticulocyte count, electrocardiogram (ECG), nasopharyngeal viral swabs, liver function tests, sputum and blood culture (tests), and other investigations needed.
It is worthy to note that, the diagnosis of acute chest syndrome is made cumbersome, as it shares the same clinical presentations with pneumonia. Infact, some sources have traced pneumonia to be the cause of acute chest syndrome.
Some of the techniques and medications employed in the treatment of Acute chest Syndrome, include:
- the use of hydroxyurea, especially for those with HbSS, sickle cell-beta zero thalassemia, and other sickle cell syndromes who experience vaso-occlusive crises,
- performing transfusion (Simple or Blood Exchange Transfusion) for the patient,
- the use of bronchodilators (commonly in adults with ACS who have asthma),
- the use of antibiotics (especially in children with ACS),
- the use of incentive spirometry,
- oxygen therapy to increase oxygen saturation.
ACS, if not well managed can lead to death. The risk of recurrence of ACS (once an individual living with SCD experiences an episode) is high. However, preventive interventions could help minimize risk. Vaccinations, asthma medications, perioperative transfusion, chronic transfusion, and hydroxyurea, are some of the measures that can help reduce the occurrence of an episode.
About Author:
Durodola Ayomide, is a student of the Lagos State University College of Medicine who enjoys reading, writing short stories, and singing. She is most passionate about creating awareness and proffering solution to sickle cell disease management, treatment and prevention, as well as other diseases. She is a young lady with great enthusiasm and resilience for a better Nigeria, Africa and Globe. Her favourite quote is that of Alfred Nobel: “For the greatest benefit to humankind.”

References:
Sickle Cell Disease Complications ( Williams’ Manual of Hematology).
ACS in SCD, by Joshua J Field, MD; Michael R. DeBaun, MD, MPH.
Acute Chest Syndrome, Wikipedia.
Acute Chest Syndrome, Sickle-cell.com.
ACS in SCD, NHS (Wessex and Thames Valley Hemaglobinopathy network).