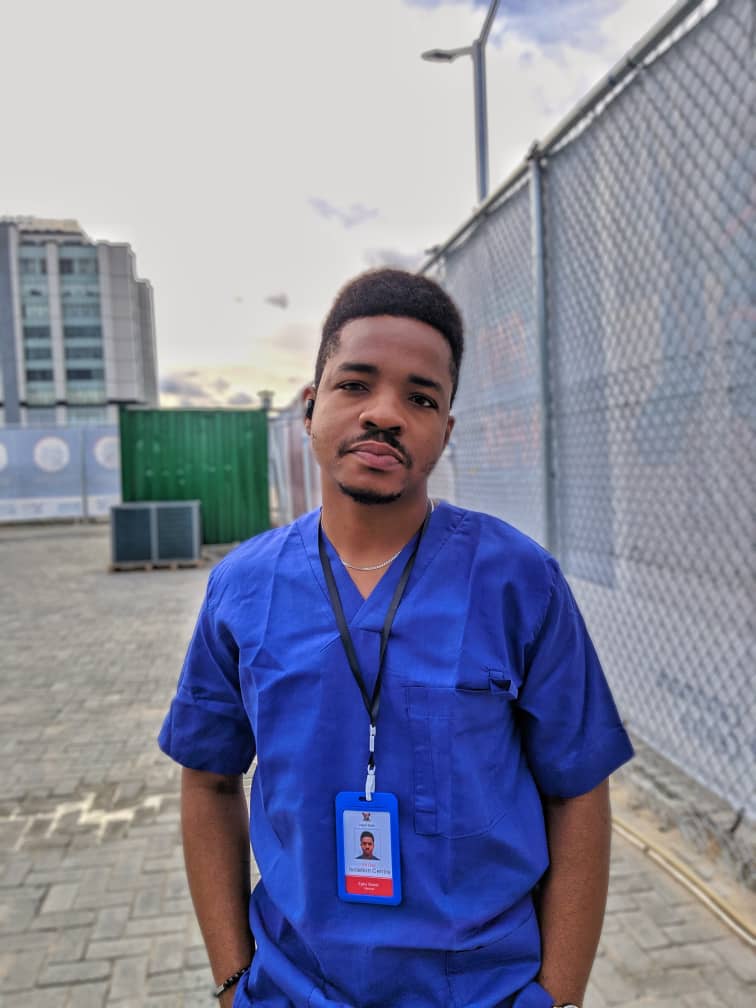
During the COVID-19 total lockdown period in Nigeria, we were privileged to speak to one of the medical officer at the Eti-Osa Isolation centre, Lagos state – Dr Egbu Sweet O., who gave us an insight into the happenings and trend of the virus spread in Lagos, Nigeria.
Dr Egbu Sweet O. is a graduate of the College of Medicine, University of Lagos, Nigeria and he describes himself as a “generation Z medical practitioner with a proclivity for clinical medicine and patient centered health care provision”. He functions based on low resolution ideas predicated to do the utmost good generally and works as a Medical Officer at the COVID-19 Isolation Centre Eti-Osa, Lagos state, Nigeria.

Q: Can you describe how the situation is like in isolation centers, especially at EtiOsa which is the epicenter in Lagos?
A: The ideal answer is difficult to articulate, because how do you put 70+ people in an enclosed environment, tell them they have a disease that has no cure, and then manage the subsequent sociocultural & quasi-dimensional unknown that comes with this new reality daily?… Think about it.
Q: Why did you decide to work at the isolation center knowing the risk attached and how dangerous it might be?
A: The correct answer is, “love for humankind”. Right? But there’s obvious empirical evidence that the individual is ultimately self-preservatory. However, when the dust settles, what will I say I was doing when my colleagues risked their lives for the preservation of society? Hence, the best way to navigate through the chaos called life, is to make a difference.
Q: Nigeria has recorded its 10,000 cases. Do you think we’re close to flattening the curve? Or the worst is yet to come?
A: It’s an old idea, that Nigerian leaders don’t have the collective responsibility and patriotism, quite frankly, to put out a body of laws, in which the absolute goal is the preservation of the general public. So, the continuous incremental direction of the disease’s statistics as of the moment, is a distinct possibility. A lot is predicated on the ethics of our choices as a society, we can only hope.
Q: Do you think our testing capabilities reflect the true proportion of those infected in the country?
A: Truth be told; we’re making the best of a suboptimal situation. but a mediocre majority of cases get noticed. Although, its actively decreasing. A lot of people don’t follow the recommended precedent, and the number of cases, while increasing, is subject to the nation’s frankly underwhelming testing capabilities. Presently, there’s over 10,000 reported cases, but there’s active community spread and most people, especially asymptomatic, don’t get tested.
Q: Can you kindly brief us on how the COVID 19 patients are being managed and what medications are currently being served at the isolation centres for the viral infection?
A: Legally, for confidentiality sake, I can’t say much but the management protocol is according to the evolving research gyrating towards the use of antiretrovirals and supportive care is pretty much standard, oriented towards the WHO COVID-19 guidelines.
Q: How is the government compensating you for your work and services? How is the hazard compensation scheme like? Is it functional? Are you lodged in hotels or asked to go home every day? Any other welfare package for frontliners?
A: The logistics in my centre is very much privately controlled. We’re compensated, obviously. Also, we’re accommodated indiscriminately for the duration of work, fed, and we have a health insurance package also covering hazards associated to the work. That’s about it.
Q: We increasingly hear news of health workers contacting the virus, what do you think is responsible for this increase and what suggestions do you have on how to reduce the prevalence knowing that Nigeria’s doctor-to-patient ratio is low pre-COVID?
A: Ostensibly, the lowest incidence of Health Care Worker (HCW) related cases happens to be in the isolation centres themselves. There’s a diastema as regards the adequate infection prevention and control measures in relation to its knowledge by HCWs across board. Also, there’s the lack of adequate training and ridiculous provision of Personal Protective Equipment (PPEs) for these HCWs outside the isolation centres. A lot of administrative policy making and government’s investment into healthcare is needed to make things better and salvage our health delivery system.
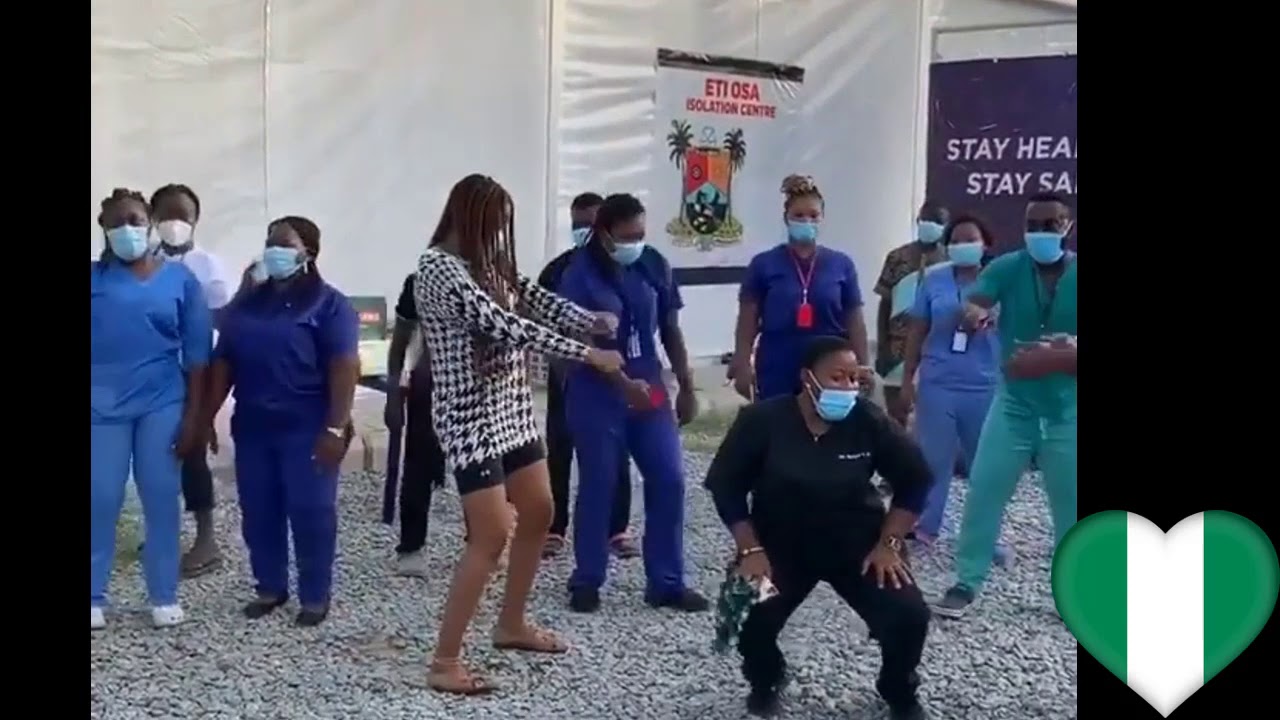
Q: People often question how real Nigeria’s COVID-19 situation is – some even say the figures are “fake” – due to circulating videos showing how patients in isolations centers are living and behaving. Some that don’t believe COVID is real ask for pictures or videos from NCDC or isolation centers. Do you think granting these requests will help educate people about how serious the coronavirus is? What can we do to instill trust in the public during this period?
A: There are ‘people’ in these centres, just like you and I, we manage them. It is however their choice to be photographed and not the public. Just like life, some people have it better than others but, there’s no doubt, “People are sick”. People have died from Sars-cov 2, societies all over the world are shut down, businesses are shut down. The human mind is very much as intriguing as it is bedazzling. COVID-19 is real
Q: In recent weeks, government at all levels have relaxed restrictions on movements despite increasing recorded cases. What are your opinions on this? What effects would this have on the citizens and healthcare systems moving forward?
A: Governments need revenue to function, hence the decision. Although, ill-timed and unnerving, the arduous decision is understandable. However, its left to us as a people to orient our new reality towards dampening the incidence of infections while moving ahead with our society. We need reappropriation of our budget to improve healthcare. Furthermore, The society will suffer, truth be told, based on empirical evidence that our government has let us down in the past.
Q: What advice do you have for Nigerians who are struggling with providing for their family and see noncompliance with social distancing or other measures as the only means to cater for their family?
A: Educate yourself to prevent getting infected, then do your best. Protect yourself. wear a facemask always, ensure the person you’re talking to is wearing a face mask. Adhere to the NCDC health guidelines. Reinvent new ways of getting valid work done. If you’re experiencing suggestive symptoms, please report to the relevant authorities.
Q: Can you share your COVID-19 experience so far with us or any peculiar story of your isolation centre successes and struggles…?
A: Imagine being a cog in the machine that’s implicitly driving away from a seemingly unyielding chaos. The general fear of day that is nested in the presupposition that the work matters. That’s the catharsis. I’ve watched people die, but I’ve also discharged a lot of people home. My heart has leaped with joy, but I also cry a lot. People ask me why I’m risking my life all the time but you know what’s funny? Patients never ask me that, they’re just really grateful.

Photo Credit – Bing.com




Discussion1 Comment
Keep up the good work