Abstract
An interstitial ectopic pregnancy is extremely rare, accounting for 2-4% of ectopic pregnancy and remains the most difficult type of ectopic pregnancy to diagnose due to low sensitivity and specificity of symptoms. We report a case of a 30-year-old woman living in Northern Nigeria (Nasarawa state) who presented to the emergency with lower abdominal pain and urinary retention of two days duration. A pelvic ultrasound revealed a Left adnexal ectopic pregnancy measuring 20.01 x 18.11mm with an intact gestational sac. An emergency laparotomy was performed revealing a massive hemoperitoneum at the uterotubal region. Postoperatively, urinary retention resolved, and the patient was discharged stable for follow up visit in the Clinic with no complications.
1. Introduction
Ectopic pregnancy refers to the implantation of a fertilized egg in a location outside of the uterine cavity {1}. Interstitial ectopic pregnancy is rare and the most dangerous form of ectopic pregnancy, accounting for 2-4% of all ectopic pregnancies {2}. Conversely, an interstitial pregnancy is a gestational sac that implants within the proximal, intramural portion of the fallopian tube that is enveloped by the myometrium.
Mahmud et al 2021 {3} presented a case of intraligamentary pregnancy with recurrent urinary retention and lower abdominal pain, where they explained the impaction of the gestational sac on the bladder could lead the atypical presentation of urinary retention. Also, two cases by Paul David et al 1999 {4} of acute urinary retention due to ectopic pregnancy proposed urinary retention as salient features in ectopic pregnancy. Furthermore, emergency physicians should consider ectopic pregnancy as a differential in any woman of childbearing age with abdominal, pelvic or urinary complaints.
Here we report a case of an interstitial pregnancy with urinary retention managed by exploratory laparotomy. However, newer methods of laparoscopy which preserve the uterine integrity for future fertility have been reported in the literature so far.
2. Case report
We report the case of 30-year-old woman who presented with a history of lower abdominal pain and urinary retention of two days duration. Her last menstrual period was 5 weeks prior to onset of symptoms.
She had no previous history of ectopic pregnancy or any previous surgeries in the past. She is a married housewife in a polygamous marriage setting. Her menarche was 14 years, and she menstruates for 4 days in a regular 28 days cycle, no history of dysmenorrhea, menorrhagia or intermenstrual bleeding. She had no history of multiple sexual partners and no history of contraceptive use. She has had two previous spontaneous miscarriage in the past.
On presentation, examination showed a middle-aged woman in painful distress, afebrile, acyanosed, not pale, not dehydrated, vitals were stable. Abdominal examination showed suprapubic fullness with associated tenderness, renal angle tenderness was positive bilaterally.
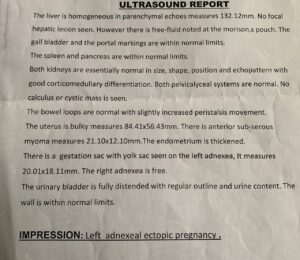
All other examinations and findings were normal. Urinalysis and Full blood count were essentially normal, Serum pregnancy test was positive. Pelvic ultrasound done revealed a gestational sac with yolk sac seen on the left adnexa measuring 20.01 x 18.11mm. The patient was counselled for an emergency exploratory laparotomy, an intraoperative finding of ruptured sac with massive hemoperitoneum around the left uterotubal junction, the ovaries was normal, and no fluid seen in the right adnexal.
A left salpingectomy was done due to the extensive damage of the tube. Postoperatively, urethral catheter was removed, and no episode of urinary retention was noted. She was placed on antibiotics and discharged to the gynecology clinic for follow up.
3. Discussion
In an interstitial ectopic pregnancy, the fertilized ovum implants in the proximal segment of the fallopian tube covered by thin myometrium with higher risk of rupturing leading to catastrophic hemorrhage than ampullary ectopic pregnancy if left undetected.
Signs and symptoms of an ectopic pregnancy are varying and include amenorrhea, pelvic pain, vagina bleeding, palpable pelvic mass, fainting spells and low blood pressure. Risk factors include previous ectopic pregnancy, abdominal or pelvic surgeries, use of an intrauterine device and pelvic inflammatory disease.
Timor-Tritsch et al {5} established 3 sonographic criteria for the diagnosis of interstitial pregnancy; an empty uterine cavity, a gestational sac located eccentrically and >1cm from the lateral wall of the uterine cavity, and a thin (<5mm) myometrial layer surrounding the gestational sac. Ackerman et al described the interstitial sign {6}.
Management include conservative approach (use of methotrexate, KCL and prostaglandins) or surgical approach based on the patient’s hemodynamic status and nature of the gestational sac.
This particular case was peculiar, in that she presented with signs and symptoms of urinary retention, which could have been as a result of impaction of the gestational sac on the bladder. Ultrasound has been shown to miss 50% of the diagnosis of intra-abdominal pregnancy, in our case two previous pelvic scan done revealed normal study. A transvaginal ultrasound which was done by a skilled radiologist revealed a left adnexal ectopic pregnancy. However, the use of Computed Tomography (CT) and Magnetic Resonance Imaging (MRI) would have provided a more accurate diagnosis.

4. Recommendation
High index of suspicion and the need for advanced imaging with qualified personnel are needed in making a diagnosis, which would have been very difficult in health facilities in Northern Nigeria due to lack of adequate diagnostic equipment and qualified personnel.
5. Conclusion
An interstitial ectopic pregnancy is a very rare life-threatening gynaecology emergency. A high index of suspicion is paramount due to varying atypical presentation and difficulty in early diagnosis. The need for advanced diagnostic equipment and skilled radiologist is important at all health facilities to avert mortality and morbidity of this condition.
6. Acknowledgement
There was no funding for this paper. Consent was taken from patient before writing of this paper.
References:
1. Ectopic Pregnancy: Practice Essentials, Background, Etiology [Internet]. Emedicine.medscape.com. 2022 [cited 28 May 2022].
2. Dagar, Mamta, et al. “Interstitial and Cornual Ectopic Pregnancy: Conservative Surgical and Medical Management.” The Journal of Obstetrics and Gynecology of India, vol. 68, no. 6, 28 Nov. 2017, pp. 471–476, 10.1007/s13224-017-1078-0. Accessed 28 May 2022.
3. Mahmoud, Salma Abdi, et al. “Intraligamentary Pregnancy with Recurrent Urine Retention: Case Report.” Open Journal of Obstetrics and Gynecology, vol. 11, no. 05, 2021, pp. 516–522, 10.4236/ojog.2021.115048. Accessed 11 Mar. 2022.
4. David, Paul R, et al. “Acute Urinary Retention due to Ectopic Pregnancy.” The American Journal of Emergency Medicine, vol. 17, no. 1, Jan. 1999, pp. 44–45, 10.1016/s0735-6757(99)90014-1. Accessed 21 May 2020.
5. Timor-Tritsch, I. E., et al. “A “Potentially Safer” Route for Puncture and Injection of Cornual Ectopic Pregnancies.” Ultrasound in Obstetrics and Gynecology, vol. 7, no. 5, May 1996, pp. 353–355, 10.1046/j.1469-
0705.1996.07050353.x
6. Ackerman, T E, et al. “Interstitial Line: Sonographic Finding in Interstitial (Cornual) Ectopic Pregnancy.” Radiology, vol. 189, no. 1, Oct. 1993, pp. 83–87, 10.1148/radiology.189.1.8372223. Accessed 28 July 2020.
Authors:
Dr. Borowa Azabi, Dr. Ibrahim Abdulqudus, Dr. Pascal Ebuka Ezerioha



