In recent times, there have been various moves and actions by the medical regulatory bodies and government of nations in Africa concerning the massive or brain drain syndrome translating into brain gain. And this has caused a lot of uproars across different levels and involved groups of healthcare workers (HCWs).
One of such was the viral picture of MDCN officials from Nigeria in October, visiting the GMC office in the UK. Another more recent case, was the news of Ghana proposing and in active engagement to exchange their trained nurses for money with foreign countries. This was announced by their Health Minister in Parliament, during the country’s 2023 Budget debate.
These different scenarios and its alarming effect on the HCWs, Healthcare system and the entire population as a whole, has increasingly made most medical associations divert their attention and resources towards discussing and proffering solutions to this catastrophic problem with an impending doom across all levels.
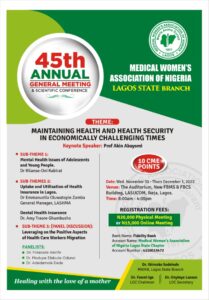
During the Annual General Meeting of one of the leading medical associations in Lagos, Nigeria – Medical Women’s Association of Nigeria (MWAN Lagos), the invited physicians on the panel discussion bewailed the state and rate of HCWs migration. Then elaborated on the need and different available means of leveraging on this migration to harness the positive gains. Some of the possible worthwhile ideas discussed are international partnership with specialists, facilities and organisations to deliver and maintain quality healthcare services through investments, innovations, provision of expertise via telemedicine or circular migration; collaboration with colleges and training institutions to provide skill acquisition and mentorship for younger medics home and abroad; also, by volunteering, actively participating in activities or keeping in touch (virtually or hybrid) with our various associations.
Interestingly, Dr. Modupe Elebute-Odunsi – Founder/CEO, Marcelle Ruth Cancer Centre and Specialist Hospital, who migrated back into the country from the UK to set up her practice mentioned that a form of brain gain that is now been experienced among quality health facilities (usually privately owned by doctors from the diaspora) is reverse medical tourism. Where they have patients from other African countries come into Nigeria to receive health care, citing an example of a patient brought in from Mozambique to receive specialist care from her facility.
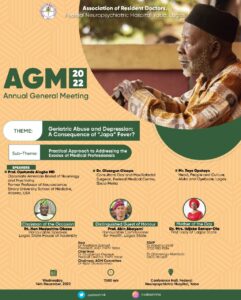
Likewise, at the FNPH Association of Resident Doctors (ARD) conference in Yaba, the depth of the healthcare system crisis caused by the Japa syndrome was explored. With the keynote speaker (Prof. O. Alagbe) highlighting the subliminal undertone of slavery and perceived exploitation of immigrant labour for the development and sustenance of those foreign countries. Also bringing to the fore that, the last wave of Japa syndrome that raged in the late 80s and early 90s was followed by the HIV/AIDS pandemic – that was mostly imported into the country from the radical globalization then. Therefore, advising that we thread with caution to avoid similar or more devastating outcomes, as well as keeping an open mind when migrating.
Japa syndrome is a colloquial term for massive migration, which occurs in the healthcare sector and beyond. It is a constellation of different signs and numerous symptoms; with a lot of push and pull factors. Japa – originally a Yoruba word translating as “to flee” – is the “flight” aspect of the normal human “flight and fight response” to an adverse situation. The adverse situation here being the critical state of the healthcare system and the general state of the Nation. Therefore, the “flight” pathway is largely chosen, because the system is difficult to fight in by any singular medical practitioner or individual.
Also, according to the panellists (Mr T. Opatayo and Dr. O. Olaopa), even though migration is inherent to man because they constantly seek for better opportunities; different opportunities abound at different times in different places. Hence, since the migration process cannot be stopped but only managed, we must begin to look on the bright side and actively work to harness the positive effect. For instance, starting up an intentional national campaign towards supporting and encourage people to come back home (beyond personal and family reasons) and invest in the nation by taking up available appointment roles, adopting facilities and so on.
“Brain drain provides space for accelerated progress for those left behind in the system, making available more opportunities to lead and excel back home. As our newly qualified doctors and trainers are going, take it as an opportunity to go out and learn, get exposure and come back to make history back home, because home will always be home” – Dr Tolu O. (Representative of the Hon. Commissioner of Health, Lagos State)
Furthermore, Dr. Olaopa touched on the issue of the abysmally low Doctor to Patient ratio in the country. Elaborating on the fact, he said that although the number of doctors available in the system is low for the WHO recommended doctor-to-patient ratio, the Nigerian healthcare sector and facilities is unable to fully utilize and reward the number that we currently have. This is reflected in the poor welfare, owed salaries of the few available doctors and the gross deficiency in healthcare infrastructure available for effective service delivery. This is usually the premise for the rhetoric statements from our ministers and politicians, insisting that we are not short of doctors. Additionally, he pleaded with doctors to avoid reacting emotionally to those statements, rather they should be juxtaposed with facts.
Recent data showed, 80% of fresh medical graduates are actively pursuing emigration and in 5 years, 50% of the population would have been successful – Dr. Olopade
Other practical solutions mentioned at the conference to cope with this massive exodus of HCWs are: providing functional welfare package and healthcare provision system for healthcare professionals; creating a clear-cut pathway for them to remain and progress in the system through residency to specialization; training and equipping more hands to provide quality care (especially for low and middle healthcare providers (e.g. TBAs) in rural areas with no formal healthcare structures or professionals); developing the concept of brain circulation or brain sharing for skill exchange through professional bodies such as West African College of Surgeons (WACS) and the likes; encouraging resource sharing through education and expansion of medical education. Likewise, citing the instance in Kenya, mental and structured support system should be created, with irresistible incentives attached to going to work in rural areas.
In a closing remark, it was stated that everyone needs to contribute to the healthcare system and infrastructure in their own little way, to achieve the positive change and effect we all desire.




